Human papillomavirus (HPV) causes the formation of papillomas, warts, warts and is a trigger in the development of cancer of the cervix and laryngopharynx. Less commonly, it can affect the oral mucosa, esophagus, conjunctiva of the eyes. According to the World Health Organization, the incidence of this infection has increased 10 times over the past 10 years. In our country the prevalence of HPV infection, according to studies in the regions, varies from 29% to 45%. The medical community is particularly wary as about one third of all isolated viral genotypes cause the development of oncological diseases.
Classification of the course of papillomavirus infection
Upon entering a woman's body, HPV can exhibit a different activity, which depends on the state of immunity. Depending on how the pathogen behaves, there are several variants of human papillomavirus infection:
- latent flow. The virus persists in the body, but does not cause pathological changes in the cells. There are no symptoms - the presence of a microorganism can only be determined using molecular biological research methods.
- Inflammation associated with HPV As a rule, we are talking about cervicitis or vulvovaginitis against the background of HPV, which lead the patient to a gynecologist. In consultation, you can find out: How to treat HPV in women. It should be understood that the virus does not cause inflammation on its own, but creates the conditions for the activation of the inflammatory process.
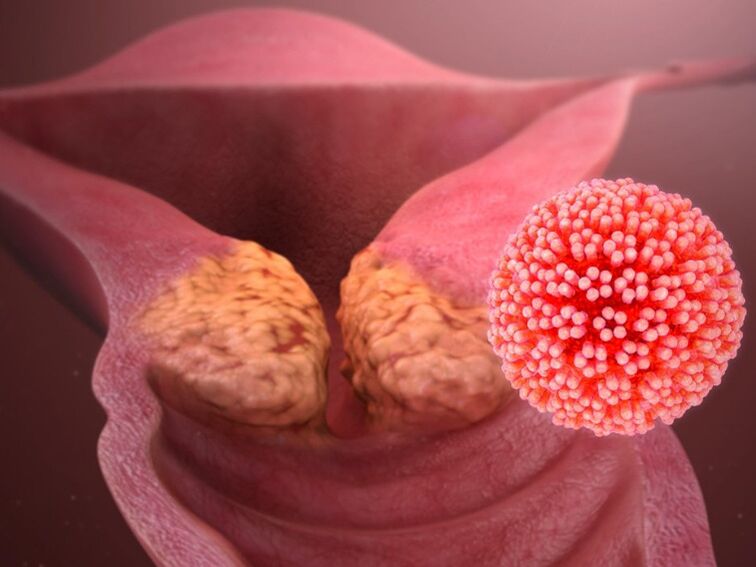
- Condylomas located in the anogenital region and on the mucous membrane of the genital tract are a form of the course of PVI (papillomavirus infection), in which it becomes necessary to use modern surgical techniques to remove the formations. After surgical removal, laser destruction, cryodestruction or radio wave coagulation, complex treatment is required to prevent complications and relapses.
- Dysplasia of the cervix. It can be asymptomatic or cause discharge. Severe forms of the disease are precancerous: to avoid this situation, a correct understanding of how HPV is treated in women is more important than ever.
The classification helps the doctor to choose the most effective treatment tactics. Pathogenic strains are also divided into groups according to their ability to cause oncological diseases: HPV with high, medium and low oncogenic risk. Among the 40 variants of the virus transmitted through sexual contact, 14 are classified as high and medium oncogenic risk: -16, -18, -31, -33, -35, -39, -45, -51, -52, - 56, - 58, -59, -66 and -68 types.
How is human papillomavirus transmitted?
Among the female population, HPV infection reaches 70%. However, the presence of a pathogen in the body does not mean a disease. If a person has a healthy immune system, the HPV infection, in most cases, is transient in nature: it goes away on its own within 2 years. If this does not happen, the question of how to treat human papillomavirus in women becomes relevant.
The main route of transmission of the virus is contact:
- sexual;
- vertical (from mother to fetus during childbirth);
- family (when using a towel, razor, underwear).
Young people between the ages of 13 and 30 are the most susceptible to virus infection. At first sexual contact, the risk of infection is about 60%. The virus can enter the body even in the absence of direct intercourse. It is girls who are most at risk for HPV, and therefore with its consequences. This is due to the peculiarities of the structure of their genital organs.
Human papillomavirus in women: causes
Among the female population, HPV infection reaches 70%. However, the presence of a pathogen in the body does not mean a disease. If a person has a healthy immune system, the HPV infection, in most cases, is transient in nature: it goes away on its own within 2 years. If this does not happen, the question of how to treat human papillomavirus in women becomes relevant.
- concomitant pathology of the reproductive system;
- endocrine disorders;
- immunodeficiencies and beriberi;
- frequent acute infectious diseases - SARS, other viral and bacterial infections;
- early sexual intercourse;
- abortions;
- smoking and drinking alcohol;
- chronic psycho-emotional stresses that weaken the immune system;
- excessive physical and emotional stress, irregular daily routine;
- postpartum period - due to stress and hormonal changes;
- long-term use of immunosuppressive drugs and oral contraceptives.
Frequent change of sexual partner also increases the risk of both infection with new strains of the virus and activation of an existing infection. If immunity is reduced, the virus is integrated into the cellular genome, which leads to a high probability of cancer: how to cure HPV in women at this stage of medical science has yet to be discovered. Therefore, it is so important to keep the activity of the virus under control and to adequately stimulate the immune defenses.
The first signs of HPV in women and additional symptoms
The most obvious sign of the presence of HPV in a woman's body is the appearance of papillomas on the mucous membranes of the genital organs and on the skin of the anogenital region. They do not cause pain and, as a rule, go unnoticed for a long time. However, the activity of the virus can provoke the appearance of other unpleasant symptoms, as a result of which a woman will immediately contact a gynecologist:
- pathological discharge from the vagina, accompanied by itching and burning;
- frequent relapses of vaginitis, bacterial vaginosis;
- foul-smelling vaginal discharge.
On examination, the doctor sees benign formations on the skin, changes in the epithelium of the cervix, signs of inflammation. Cancer can only appear in the later stages of a chronic papillomavirus infection.
Is there a cure for human papillomavirus?
To understand how HPV is currently being treated in women, it is necessary to understand what approaches exist in the treatment of human papillomavirus infection. At present, the therapy of HPV infection boils down to the following activities:
- prevention of the progression of HPV infection;
- elimination of clinical manifestations;
- stimulation of systemic and local antiviral immunity.
There are no drugs that lead to the complete disappearance of the virus from the body. However, research in this area is ongoing: the attention of doctors is focused on the need for combined treatment of various manifestations of HPV. Research in genetic engineering is promising. Scientists are exploring the possibility of "rewriting" the viral code to self-destruct instead of spreading. The reduction of viral copies restores local immunity and eliminates chronic inflammation.
Information for physicians on "How to treat HPV in women" is currently detailed in current clinical guidelines.
When is it necessary to see a doctor?
Women should undergo a preventive examination by a gynecologist at least once a year. Also, the need to visit a doctor arises when disturbing symptoms appear:
- neoplasms in the genital area;
- warts on other areas of the skin and mucous membranes;
- pain in the lower abdomen;
- unusual discharge or foul odor from the vagina;
- itching, swelling, redness of the genitals.
In a situation where accidental sexual intercourse has occurred, it is recommended to visit a gynecologist. She will conduct an exam, take a gynecological smear, and scrape to detect HPV.
If papillomas occur in other parts of the body, a consultation with a dermatovenereologist is required. When papillomas or warts grow in the anus, the intervention of a proctologist may be required. This will help determine the tactics of treatment and what remedies for papilloma should be prescribed to the patient in a particular case for purchase at the pharmacy.
General therapy scheme
The main weapon in the fight against HPV is the stable immunity of the person himself. The American Center for Disease Control and Prevention draws attention to the fact that in 90% of cases of contact with the virus, clinical manifestations do not develop due to the self-suppression of the virus by natural immunity.
Treatment for HPV infection should be comprehensive and aimed at:
- therapy of concomitant diseases;
- elimination of external manifestations of diseases - medically and, if necessary, surgical;
- reduction of viral load;
- stimulation of the body's own defenses.
Chronic psycho-emotional stress, poor environment, and comorbidities reduce the ability of a woman's immune system to cope with the virus on its own. There are drugs that, having a direct antiviral and immunomodulatory effect, help the body's strength and lead to a decrease in viral load. These modern drugs include a spray with activated glycyrrhizic acid, made from licorice root. It helps stop the early replication of the virus and reduces the number of copies of the HPV genetic material in the body. The tool has a special intravaginal nozzle for administering drugs to the cervix and its uniform distribution along the walls of the vagina. Antiviral and immunomodulatory therapy in the latent course of papillomavirus infection can prevent the appearance of unpleasant symptoms and the transition of the infection to more aggressive forms. If the virus has caused changes in the genital area and cervical epithelium, the spray helps:
- relieve inflammation;
- eliminate itching;
- restore the integrity of the mucous membrane;
- increase local immunity.
The use of the product is also indicated in the preparation period for the removal of benign formations caused by HPV, to reduce the activity of the virus and prevent relapses. The drug helps to regenerate the skin and prevent the attachment of a secondary infection.
Removal of papillomas and warts
Benign formations caused by HPV are subject to removal, which can be done by the following methods:
- cryodestruction - exposure to neoplasm with cold;
- electrocoagulation - treatment with high frequency current;
- laser removal - layer-by-layer exposure to laser irradiation until a crust appears;
- chemical destruction - treatment with special chemical solutions that are applied to warts and destroy them;
- surgical removal - given the high risk of relapse after this type of destruction, it is selectively prescribed - if it is impossible to use other methods.
Among the new developments in the treatment of HPV is the CRISPR / Cas9 system, which almost completely cuts the DNA and incorporates its sections, thus inactivating the further spread of the virus.
Prevention
For primary prevention, the use of barrier contraceptives (condoms) is recommended, which, while not absolute protection against HPV, will reduce the level of exposure to the virus. You should be selective in choosing your sexual partners. If an accidental connection has occurred, a special spray can be used to protect against infection with HPV, herpes simplex virus and cytomegalovirus.
To date, HPV vaccination is the most effective. It protects against the most common and malignant types of human papillomavirus. In many countries, HPV vaccination is included in the mandatory vaccination calendar. The most effective time for vaccination is in childhood and adolescence. Previously, it was believed that after 20 years of vaccination it makes no sense. But recent studies have shown that HPV vaccination is appropriate and effective up to the age of 45-47.
If a virus infection occurs, the task of secondary prevention is to maintain the patient's good health, especially the good state of his immune system. Women should visit a gynecologist regularly to detect virus-associated diseases in the early stages.
















































































